How epidemiology detectives are tracing each Alaska coronavirus case
How epidemiology detectives are tracing each Alaska coronavirus case By Michelle Theriault Boots, Anchorage Daily News, April 17, 2020
Every time an Alaskan tests positive for the coronavirus, a small army of nurses leaps into action, launching public health investigations known as “contact tracing.”
Before the new coronavirus, Bethany Zimpelman was an elementary school nurse, tending to her Muldoon Elementary students’ playground injuries and primary care.
Now she is a public health detective of sorts, following an invisible web of coronavirus infections.
Every time an Alaskan tests positive for the coronavirus, a small army of nurses like Zimpelman leaps into action, launching the virus investigations known as “contact tracing.”
In Alaska, each person with a confirmed positive coronavirus case — more than 300 as of midday Saturday — has gone through the contact tracing process, said Joe McLaughlin, Alaska’s state epidemiologist.
Contact tracing involves sussing out all close human contact an infected person has had during their infectious period, creating a detailed timeline of their daily life in order to identify and advise the people exposed that they need to self-quarantine or isolate, in hopes of arresting the chain of transmission spreading the virus, said McLaughlin.
It is low-tech, detail-heavy work that involves asking strangers probing questions by phone for hours at a time, and methodically checking back with exposed people to ask about their symptoms, nurses say.
Alaska public health officials say it’s one of the best weapons they have in corralling the coronavirus.
“Every single person who has tested positive for coronavirus has had this tracing process done,” said Tim Struna, the Juneau-based head of the Division of Public Health’s statewide public nursing section. “It is part of what’s keeping the curve down in Alaska.”
Projected exponential growth in coronavirus cases in Alaska has not materialized, said Struna.
“I think that can be attributed to these two strategies: People in Alaska doing the best they can to social distance,” he said. “And the contact tracing.”
On Wednesday, Alaska’s chief medical officer Anne Zink called “aggressive contact investigations” one of a handful of practices that could stop localized outbreaks. The following day, she suggested that Alaskans keep a log of daily interactions to make it easier for public health workers to track down who they may have been in contact with if they were exposed to the virus.
Contact tracing is a core tool in epidemiology, used for everything from identifying tuberculosis clusters to measles outbreaks. Even before the coronavirus pandemic, Alaska’s public health nurses already did a lot of it, perhaps spending a quarter of their time tracking exposures, said Struna. Now they are spending 70% of their time on it, he said.
There is no point in an outbreak at which contact tracing really becomes irrelevant, Struna said.
“I would say it always matters,” he said. “If there’s widespread transmission and we still have a workforce that can keep up with the contract tracing, we’re going to do it until the end.”
Asking questions
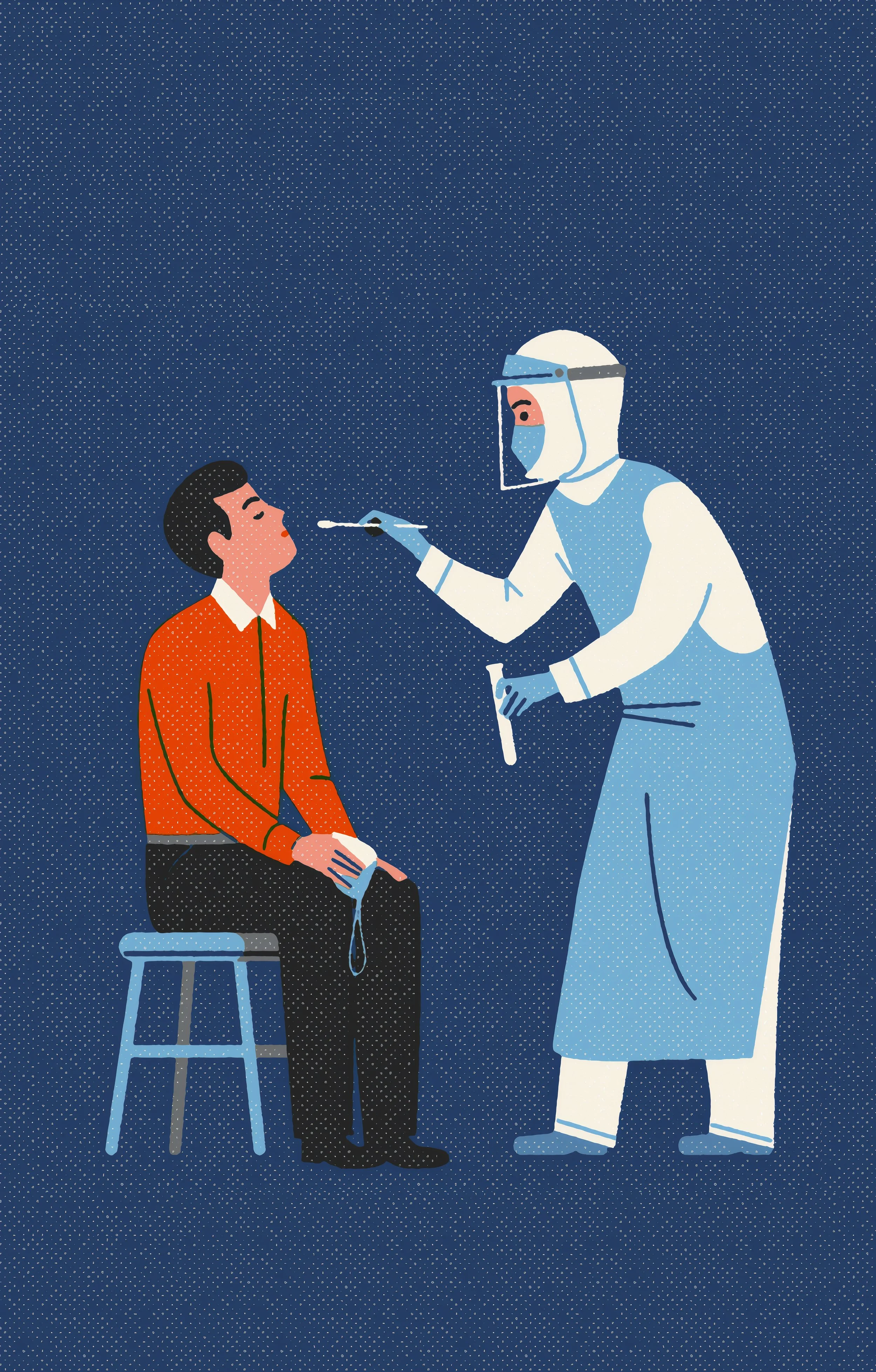
Here’s how the process works: When an Alaskan tests positive for COVID-19, nurses get on the phone.
Most of the people doing contact tracing are public health nurses scattered across the state. Anchorage is handling its own tracking for cases within the municipality, using a few nurses employed by the city health department supplemented with dozens of volunteer Anchorage School District nurses, drafted to help after schools shut down, said Art Tovar head of the community health nursing program for the Anchorage Health Department.
The nurses received a two-hour training, said Jennifer Patronas, head of health services with the Anchorage School District.
“They love it,” said Patronas. “We started with five nurses doing it, volunteering for it. One of those nurses started a Zoom meeting, and they were sold. Now all of them want to do it.”
Usually, a person who tested positive has already been informed of the test result by their medical provider. The next phone call they might receive is from a contact tracer.
Nurses ask questions to build a timeline of the person’s sickness, determining their period of infectiousness -- when they are most likely to be shedding the virus in respiratory droplets or other secretions. For the novel coronavirus, that infectious period is generally thought to be two days prior to the first symptoms to at least seven days after the onset of the illness, said McLaughlin, the state epidemiologist.
Then comes the part that makes contact tracing more like a detective’s investigation: “We ask them to try to recall each and every person they came into contact with during that infectious window, and the nature of the contact, and the duration of the contact,” McLaughlin said.
It’s a tall order, said Zimpelman.
“Fourteen days is a long time to remember,” she said.
Many people are initially foggy when asked to recount every detail of their day on the spot, said Struna.
So nurses are trained in the painstaking process of asking probing questions: On Monday, did you leave your house? Where did you go? How did you get there? Did you travel with anyone there? Did you talk to anyone when you got there? How did you travel home?
Repeat that for every single day, and you’re starting to catalog a comprehensive list of close contacts, Struna said.
Sometimes nurses ask people to use their phones or calendars to jog their memories about what they’ve been doing — who they’ve been texting, where they’ve been spending money.
“We have people re-track their bank statements, their credit cards. Sometimes moms, especially, will be taking pictures — they have like a little journal on their phone,” Zimpelman said.
With every phone call Zimpelman makes, she learns where the virus may have wandered: to a grocery store, a workplace, a park.
“Each phone call makes it kind of grow exponentially,” she said.
In some cases where exposure within a public place or institution is suspected, other data can be used, McLaughlin said: Medical offices can provide chart information, prisons can share video footage, businesses can share transaction records and airlines could offer passenger manifests.
The conversations can take an hour or more, said Tovar.
In general, the quality of the contact tracing information relies on the person’s willingness to volunteer it to a nurse.
People are not always forthcoming, Zimpelman said. People feel fear and stigma when they hear they have the virus or may have been exposed, she said.
“You’re trying to work with them as non-judgmentally as possible, and protect their privacy,” she said.
‘10 minutes within 6 feet of a person’
Getting an accurate and complete timeline of the infected person’s contacts is crucial to the next step of contact tracing: letting all of the “close contacts” know they have been exposed to the coronavirus.
Prolonged exposure, by the state’s definition, is “10 minutes within 6 feet of a person,” according to McLaughlin.
In most cases, that rules out casual interactions such as standing in line at Costco or passing in the aisle of a Fred Meyer — unless the infected person directly sneezed or coughed on someone, he said.
“For COVID-19 we are really looking for more prolonged interactions than passing someone at a grocery store,” he said.
Social distancing measures have winnowed the number of potential close contacts most positive cases report, McLaughlin said. Best case scenario, a person with COVID-19 only has three or fewer close contacts, possibly just household members, he said.
People who’ve been out and about, or going to work, could have exposed many more. Anything over 10 close contacts is “a lot, in my mind,” he said.
If you’re identified as a close contact of a person with coronavirus, your name goes on a list of people being monitored, according to McLaughlin.
Then a nurse calls you, lets you know you’ve been exposed, and tells you to self-quarantine for 14 days and closely watch for virus symptoms, he said.
If the person cannot be reached by phone, nurses will go to their houses — wearing protective equipment — to inform them. Some nurses have also dropped off masks, thermometers and other quarantine necessities, said Tovar of the Anchorage Health Department.
For people whose living situations don’t allow for quarantine conditions, nurses might also try to help them find suitable housing. Nurses check back in daily until the end of the 14-day period. If a person develops symptoms, nurses instruct them to get tested, according to McLaughlin and Struna.
If someone refuses to quarantine, the state can file a court petition to order them to do it. That hasn’t happened yet, said Mara Rabinowitz, a spokeswoman for the Alaska Court System.
“People are generally compliant. Everybody knows we’re in the middle of a pandemic,” said McLaughlin.
So far, Zimpelman and the other nurses have made many hundreds of calls to untangle the threads of interaction that could have led to infection — or that could lead the new ones. They’re asking people what their temperature is. And with each call, Alaska comes a little closer to understanding the scope of the coronavirus.
“I feel lucky to be doing this right now,” she said.