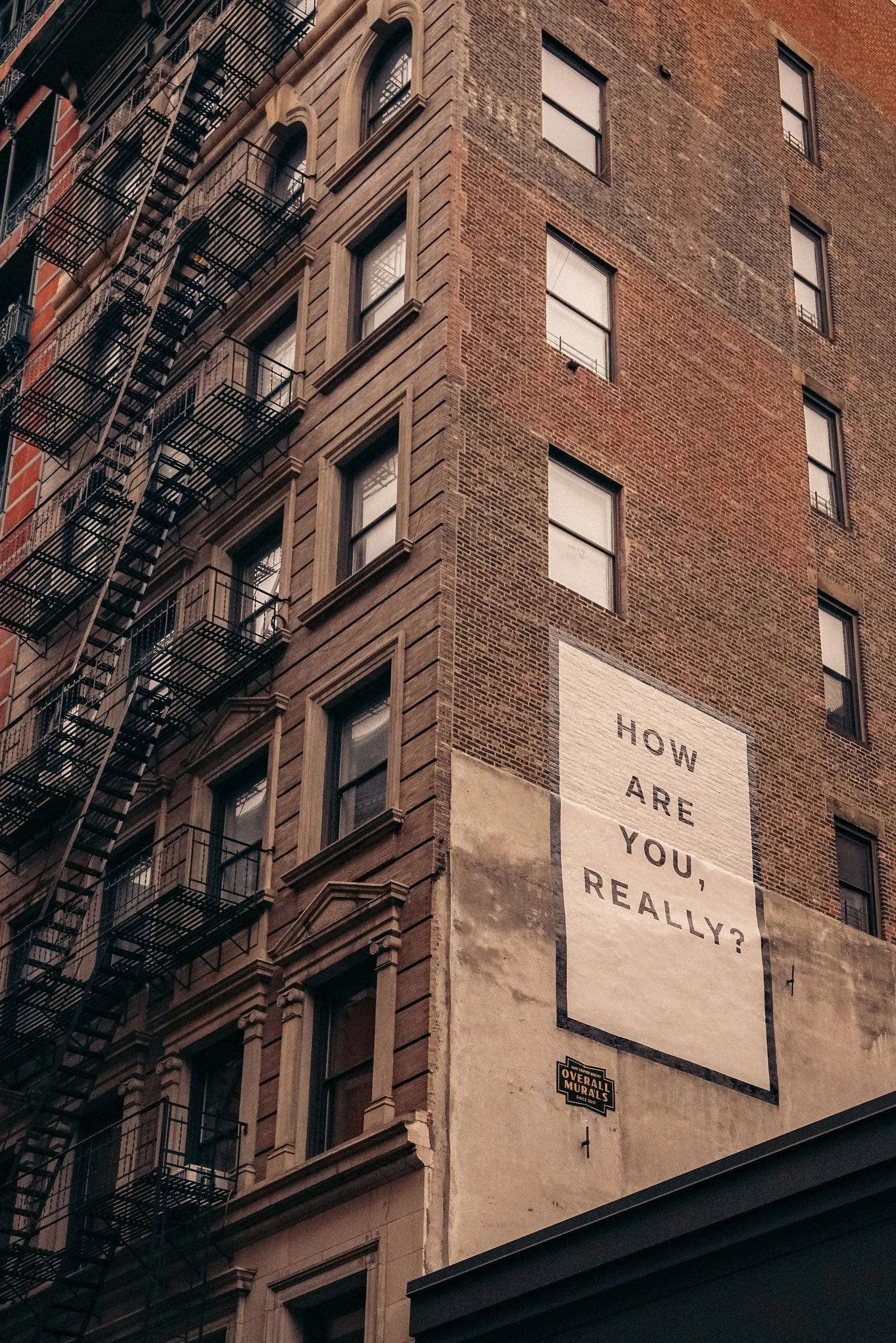
How Cities Are Addressing Mental Distress
How Cities Are Addressing Mental Distress
By Kate Elizabeth Queram, Route Fifty, November 18, 2021
word count: 1054
The Covid-19 pandemic exacerbated existing trauma and mental-health issues in vulnerable populations across the country. But the ubiquity of those issues—and the spotlight trained on them as communities continue to recover from the pandemic—presents a unique opportunity to implement new solutions to address them, municipal leaders said Wednesday at the National League of Cities Virtual City Summit.
“We are at a watershed moment culturally, and we can’t let this moment pass us by,” Barbie Robinson, executive director of Texas’ Harris County Public Health, said during a panel discussion. “I often talk about how the lack of parity and access to mental health services is one of the greatest civil rights issues of our times. If you couple that with who has access, and what are the drivers of trauma and mental health issues, and with racism being such a huge driver...we cannot let this moment pass us by.”
Robinson was one of four experts on a panel convened to discuss emerging local solutions for addressing trauma and mental health challenges, both in specific populations and across communities. Getting a handle on the problem, panelists said, is a complex mix of gathering data, establishing outside partnerships and learning to listen—really listen—to what struggling residents say they need.
In Pittsburgh, for example, first responders were experiencing a common problem—police and paramedics were frequently being dispatched to help people in mental distress, situations they are usually ill-equipped to handle.
A traditional solution is the use of embedded behavioral health teams composed of social workers or counselors who accompany police on mental wellness calls. But in Pittsburgh, city officials tried something different: They asked the first responders what would help.
“Fire, police and EMS are so often in these positions of, ‘Just do what you’re told. Don’t tell us what’s wrong, just go back out and do it some more,’” said Laura Drogowski, manager of the newly created Office of Community Health and Safety. “It’s exhausting, it’s burning them out and it’s harming our communities. Our first responders needed help. If you talked to any single one of them, they said, ‘We need help. We don’t want to do this.’ But when you call 911, you’re getting fire, police or EMS.”
City leaders listened to the feedback and then tweaked existing services to fit the problem. Data was key to that process, Drogowski said, including one metric showing that 30% of overdose victims were declining transport to emergency departments.
“They weren’t treated well in those departments,” she said. “They felt like crap, and they didn’t have transportation home.”
One possible solution, she said, is a program that allows responding paramedics to distribute buprenorphine—a medication for opioid-use disorder–alongside the overdose-reversing drug naloxone, with the hope of easing physical pain to potentially allow users to more clearly assess their options.
“It helps that person feel better and perhaps access treatment if that's what they choose to do,” she said. “But we wouldn’t know any of this if we hadn’t listened.”
Those conversations happen throughout Pennsylvania’s Allegheny County, between police, mental health professionals and members of vulnerable populations, including homeless residents, said Daniel Palka, director of urban health and street medicine for Allegheny Health Network, which partners with the city to integrate mental health services into emergency response.
“The individuals we work with would bemoan and lament the poor interactions they had with public safety, and on the other side, the public safety professionals would also say, ‘That was a horrible interaction,’” Palka said. “So we got them together and said, ‘What do we need?’”
The answer, they said, was more people on the ground, trained to spend the time necessary with individuals in distress and to prioritize what’s known as “unconditional positive regard,” or complete acceptance and support of people in need.
Traditional public safety workers aren’t equipped for those types of interactions and often lack the time or desire to be trained to do so, Palka said. But counselors and social workers could potentially learn to respond to incidents the same way that police do—quickly, reliably and on the scene, meeting people where they are.
“If we can show up just like they do and bring that unconditional positive regard, we can absolve public safety of trying to understand which shelter has a bed that’s open right now, or what it is about this person’s psychiatric condition that’s created a behavioral issue on the street,” Palka said.
The partnership launched in April in three zones throughout the city and has so far completed more than 500 calls in cooperation with public safety. Police have “wildly accepted” the program, Palka said, and their relationships with the mental health professionals have led to a more open exchange of information regarding the outcomes of specific cases.
“They want to know it resulted in something positive, so just being able to have a case conference with public safety is huge,” he said. “We don’t have to disclose protected health information, but we can say, ‘Hey, this person is now in a housing placement.’ It’s made a world of difference to those officers participating in the program.”
Other Ways to Address Mental Health Issues
Barriers to mental health resources can be addressed in smaller ways as well. In Baltimore, officials noticed that a restriction in the city’s application process prevented formerly incarcerated residents from participating on boards and commissions—including one designed to address the challenges of newly released inmates.
“We started the wheels turning from the internal parts of government to get it shifted and really found out that we can do what we want to do,” said William Kellibrew, director of the city health department’s Office of Youth and Trauma Services. “We had the website changed so that restriction wasn’t there...and it did not take the city council to remove it. It just took asking, ‘Well, why do we have it on there as a barrier in the first place?’”
Regardless of the specifics of an individual program, panelists agreed that successfully addressing trauma and mental health in a community typically relies on a format that incorporates the larger structural forces and social determinants of health, including racism and poverty—a process known as “looking upstream.”
“Someone doesn't just end up in that situation,” Drogowski said. “There’s a whole bunch of things that don’t come together, and services that ultimately fail them.”